Free shipping on all orders over $50 | Subscribe & save 15%
Free shipping on all orders over $50 | Subscribe & save 15%


During the transition to perimenopause and eventually menopause, the female body undergoes hormonal changes due to declining hormone levels. These can cause a variety of not-so-pleasant symptoms such as hot flashes, brain fog, and decreased libido. While these symptoms are all widely known to be associated with (peri)menopause, bladder symptoms are also extremely common. Symptoms such as urinary frequency, urinary urgency, pain with urination, and urinary tract infections (UTIs) or feeling like you have UTI when you don’t, fall under the condition known as genitourinary syndrome of menopause (GSM). So let’s dive into the science behind treating ‘menopause bladder’.
Embryologically, the lower urinary tract (bladder, urethra), vulva, and lower vagina are derived from the same place: the urogenital sinus. Because of this, these tissues respond to estrogen… and lack of.
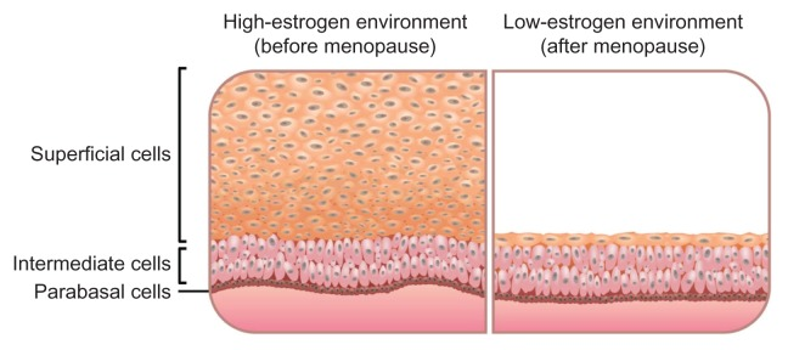
With decreasing estrogen levels, the vaginal tissue thins. This can result in vaginal dryness with associated painful sex, but it can also result in recurrent UTIs.
The reason this occurs is because the superficial cells of the vagina provide food for the Lactobacilli bacteria which are the “good” bacteria. The Lactobacilli bacteria help maintain an optimal pH in the vagina by producing lactic acid. This slightly acidic environment is optimal for Lactobacilli, but inhibits growth of other organisms such as pathogenic bacteria and yeast. When the vaginal lining becomes thin, there are lower numbers of Lactobacilli. Thisresults in an overgrowth, or proportionately higher number of harmful bacteria that can cause UTIs.
Low estrogen also makes the bladder lining more sensitive. This causes symptoms of urinary frequency, urgency, and even loss of urine with an overwhelming urge to urinate (urge incontinence). Some women may have a burning sensation, which may be misdiagnosed as a UTI, and treated with unnecessary antibiotics. These antibiotics can further disrupt the already impaired vaginal microbiome, thus aggravating the symptoms of GSM and complicating the treatment of ‘menopause bladder’.
Since lack of estrogen seems to be the problem, then estrogen treatment is the solution. Topical estrogen is the gold standard of treatment for GSM because it gives targeted relief without systemic effects. But what if you don’t want to take estrogen? Or you still have symptoms of GSM despite taking estrogen and want a non-prescription option? That’s when Femetry’s bladder supplements can help.

Femetry 1 is Bladder Flora Balance. It contains over 10 billion colony forming units (CFUs) of three different types of probiotics. Probiotics are another word for beneficial bacteria, often given in supplement form, to help restore and maintain the body’s natural microbial function.
Lactobacillus acidophilus is well known as an effective probiotic, particularly for gut health. However, it is also supportive to bladder and vaginal health! In a randomized, double-blind, placebo-controlled clinical trial, L.acidophilus was found to significantly reduce menopausal symptoms in women aged 40-601. Another study showed that it was even more effective in reducing UTIs in menopausal women when combined with D-mannose and inulin, both in Femetry2!
The other Lactobacilli strains are L. reuteri and L. rhamnosus which are the most clinically studied strains for urinary tract health. Unlike L. acidophilus which exists predominantly in the gut, L. reuteri and L. rhamnosus are found primarily in the vaginal and urinary epithelium. Together, they help restore the normal vaginal microbiome in menopausal women, inhibiting yeast and bacterial pathogens. They have also been found in clinical trials to reduce the recurrence of UTIs3.
And while Femetry 1: Bladder Flora Balance actively addresses the urinary tract’s defense mechanisms to fight off infections and irritation, Femetry 2: Bladder Daily Comfort works by calming the inflamed bladder and replenishing the bladder wall itself. Ingredients including quercetin, rutin and aloe vera are all antioxidants and are naturally anti-inflammatory. These soothe and reduce oxidative stress and damage to the bladder tissue, promoting a healthy histamine response.
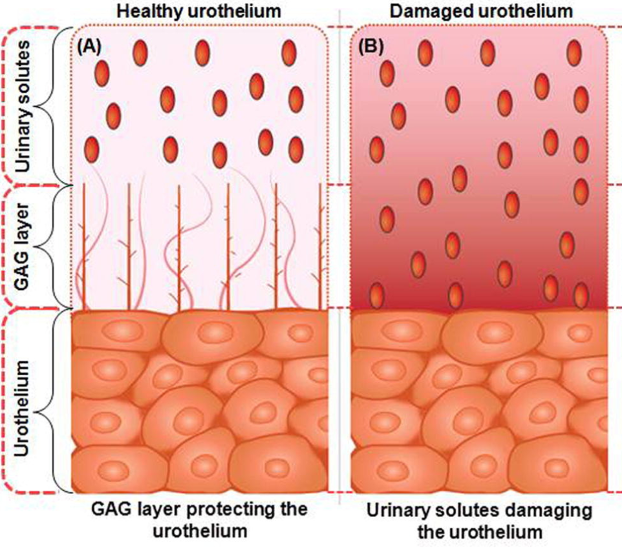
Other ingredients provide the building blocks for the protective layer of the bladder inner lining, also referred to as the glycosaminoglycan (GAG) layer. Hyaluronic acid itself is a glycosaminoglycan, aloe vera contains GAGs, and quercetin can stimulate the production of GAGs. Together, these components help rebuild and fortify the GAG layer that functions to prevent irritating toxins in the urine from coming into direct contact with the sensitive bladder tissue.
Furthermore, it contains Ashwagandha which has been used for centuries in traditional Indian medicine to reduce cortisol levels. Not only can that have a significant impact on immunologic response, it can also reduce the stress and anxiety related to having bladder conditions, such as avoiding intimacy due to fear of getting a UTI and avoiding social situations for fear of certain food or drink triggering bladder pain.
You don’t have to be in menopause to have GSM symptoms. Decreased levels of estrogen can happen to women of all ages due to a variety of reasons. For example, medications such as low dose oral contraceptives or breast cancer treatments can cause decreased estrogen levels. Breastfeeding can suppress estrogen production, as can ovarian issues and even thyroid disease. And because Femetry is a non-hormonal supplement, regardless of what causes your symptoms, Femetry can help!
Whether you are premenopausal, perimenopausal, or menopausal, if you are dealing with recurrent UTIs, urinary frequency, or bladder discomfort, Femetry might be just what you need.
