Free shipping on all orders over $50 | Subscribe & save 15%
Free shipping on all orders over $50 | Subscribe & save 15%


Menopause is a natural transition in a woman’s life, often accompanied by a range of symptoms—from hot flashes to mood swings. However, one lesser-known yet very common consequence is Genitourinary Syndrome of Menopause (GSM). Despite affecting up to 80% of women, GSM often goes undiscussed due to stigma or lack of awareness.
What is Genitourinary Syndrome of Menopause?
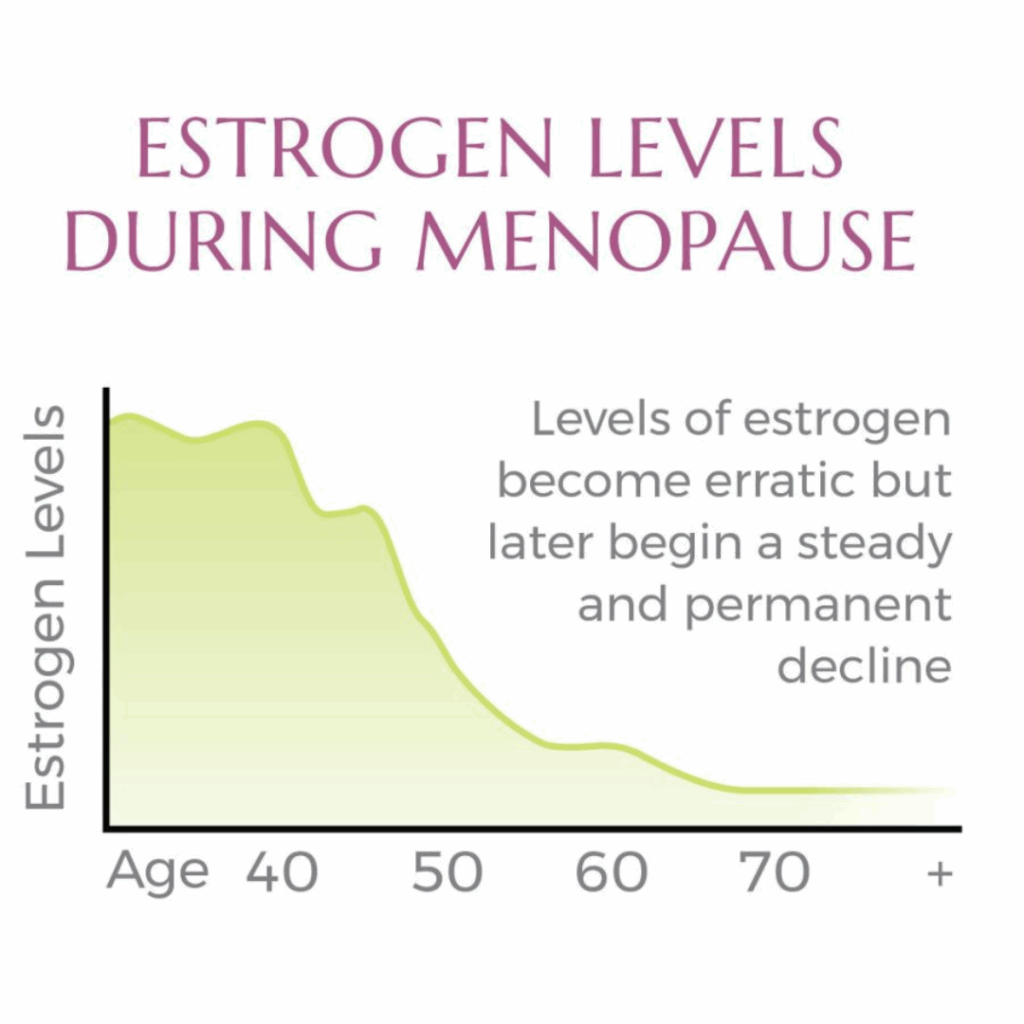
Genitourinary Syndrome of Menopause (GSM) refers to a collection of symptoms and signs resulting from the decline in estrogen levels during and after menopause. This drop in estrogen affects the vulva, vagina, urethra, and bladder, leading to a range of uncomfortable and disruptive symptoms.

Common Symptoms of GSM
Vaginal Symptoms:
Urinary Symptoms:
These symptoms can significantly impact a woman’s quality of life, sexual health, and emotional well-being.
GSM primarily affects women in perimenopause or who are postmenopausal, typically starting in their 40s or 50s. However, it can also affect:
Why Does GSM Happen?
The primary cause is a decline in estrogen, the hormone responsible for maintaining the health of the vaginal and urinary tissues. When estrogen levels fall:
How is GSM diagnosed?
GSM is typically diagnosed through a clinical evaluation, which may include:
Unfortunately, many doctors have not been trained to ask about symptoms of GSM, so it is important to discuss them with your doctor if they become bothersome.
How is GSM treated?
Fortunately, GSM is treatable. Management depends on the severity of symptoms and the individual’s medical history.
1. Non-Hormonal Treatments
2. Hormonal Treatments
3. Supplemental Therapies
Many women hesitate to talk about GSM due to embarrassment or the belief that symptoms are an inevitable part of aging. But you don’t have to suffer in silence. Talking to a gynecologist, primary care provider, or a menopause specialist can lead to effective treatment and a better quality of life.
Genitourinary Syndrome of Menopause is common but not something you have to just live with. Recognizing the symptoms and seeking appropriate care can make a significant difference in comfort, health, and overall well-being during and after menopause.
GSM and IC
GSM can exacerbate or mimic IC symptoms. As previously mentioned, the thinning of vaginal and urethral linings decreases elasticity and blood flow which may cause urethral or vaginal burning and irritation. Estrogen also plays a role in maintaining the integrity of the bladder lining, so decreased estrogen may impair the strength of the bladder lining, increasing urinary urgency, frequency and possibly bladder pain. If are perimenopausal or postmenopausal and have IC, it is always a good idea to discuss with your doctor whether or not you would benefit from vaginal estrogen or GSM treatment.
Resources:
