Free shipping on all orders over $50 | Subscribe & save 15%
Free shipping on all orders over $50 | Subscribe & save 15%


Pelvic floor physical therapy includes techniques, such as stretching and the release of tight muscles, that could help ease pain for many patients with Interstitial Cystitis (IC).
Chances are, you’re familiar with physical therapy, or PT. PT is commonly used to help with discomfort for an ankle or knee injury, for example.
Many patients with IC have tenderness or tension in the pelvic floor muscles, which surround the bladder. It is unclear whether this pelvic floor muscle pain occurs as a result of IC, or if the muscle tension and pain in the pelvic floor muscles is what causes the bladder pain and IC. Nevertheless, research has shown that pelvic floor PT, including stretching and the release of these tight muscle bands and scar tissue, can help relieve pain for many patients with IC.
A helpful analogy is to think about squeezing your hand muscles in a tight fist. Can you imagine the amount of pain you’d be in if you did that for several months? A similar process occurs in pelvic floor muscles when people develop stress and tension in this area of the body.
For many people with IC, this results in significant pain that could be eased by exercises that allow release of this tension from the muscles.
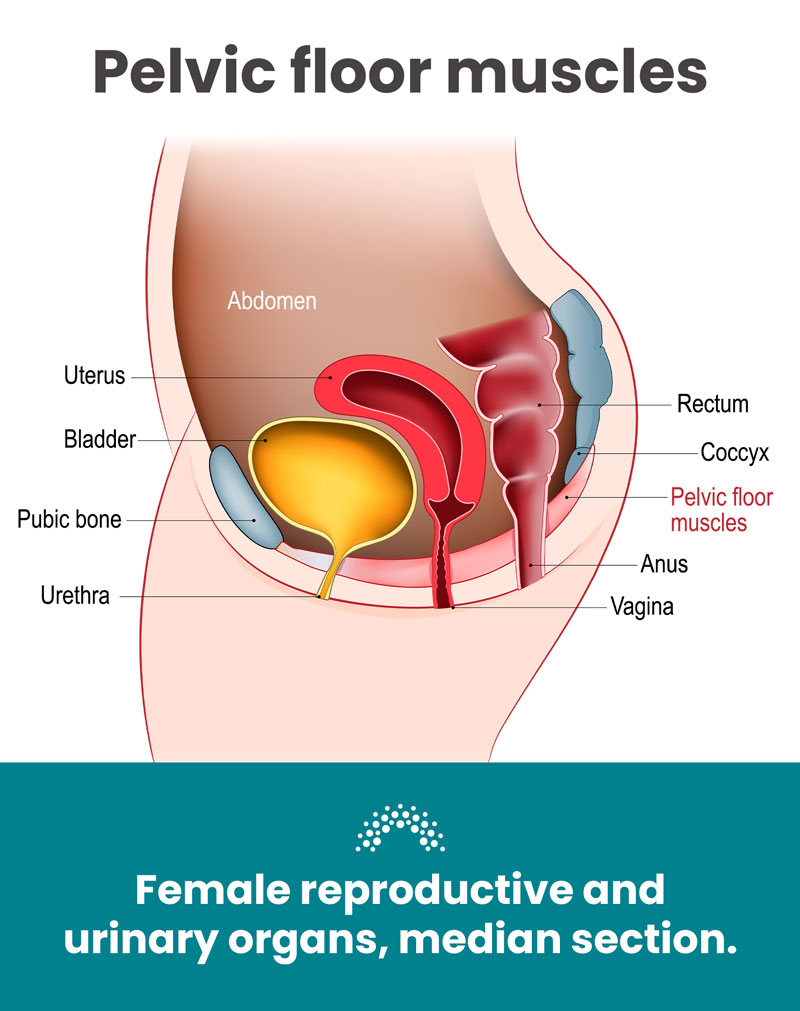
The pelvic floor consists of muscles and connective tissue that stabilize your core. It also supports your pelvic organs, which include your bladder, urethra, vagina, uterus, rectum, and intestines.
The pelvic floor is even responsible for control over bodily functions, including peeing, pooping, and sexual intercourse. Many people with pelvic floor muscle problems have a difficult time relaxing and coordinating their pelvic floor muscles appropriately. We call this “pelvic floor muscle dysfunction.”
Pelvic floor PT is helpful for people with IC and many other types of pelvic floor disorders. If you have pelvic floor tenderness, it may be especially helpful. For instance, if someone feels pain whenever their doctor does an internal exam and touches anywhere in the vaginal canal, they may have generalized pain in the pelvic floor muscles.
Similarly, if you have pain in one specific area, this is commonly referred to as a “trigger point.” Another indication that you could benefit from pelvic floor PT is if you have pain during sexual intercourse.
The goal for this form of physcal therapy is to balance your muscle strength and tension. The type of pelvic floor PT that is done for people with IC is focused on relaxing the pelvic floor. This differs from exercises that strengthen the pelvic floor.
It is important to remember that if you have IC or pelvic pain, you probably do not need Kegel exercises or pelvic floor muscle strengthening. This type of exercise can make your bladder pain worse. Exercises to strengthen the pelvic floor are used for women with urinary incontinence (leaking urine) or pelvic organ prolapse (dropping of pelvic organs out of the vagina).

Pelvic floor PT is very specialized. That’s why it is important that you make an appointment with a physical therapist who has specialized training in treating pelvic floor conditions. The first appointment typically consists of an evaluation of your health history and experience with IC. Your physical therapist will also include some education about anatomy and how PT works.
The physical therapist will then perform an external and internal exam. Some people prefer to wait for the second visit to perform the exam. This will give you time to get to know each other and gain trust in the first appointment. If you would prefer to wait for the exam, make sure to mention it!
The internal exam will be similar to a pelvic exam. However, the PT’s internal exam will involve the insertion of only a gloved finger into the vagina for women (and not a speculum). Physical therapists will be feeling for muscle tone, evaluating for locations of pain, and evaluating muscle control.
After the exam, your physical therapist will come up with a plan for you. This plan should include work you do together during your sessions and at home by yourself. Your plan might include the following:
Nope! You don’t need anything for your appointment with a physical therapist. However, you will probably want to wear loose fitting clothes so you are comfortable.

The internal exam and the first few sessions may be uncomfortable if you have a lot of pelvic floor muscle pain. It’s a good idea to schedule the first appointment at a time when you may have a lower threshold for pain. Try to book when you are not having a flare of IC symptoms or on your period.
Over time, each session should get easier and less painful. You may consider asking your doctor or pelvic floor physical therapist for a topical lidocaine gel to use before internal work. This may make the area slightly numb and decrease pain.
All in all, physical therapy could be helpful for your IC-related bladder pain. Remember, it’s so important to cater your relief options to your body and find out what works for you.
Femetry and your “Down There” Doctors are here to support you! For more informative blogs, resources, and support, subscribe to our newsletter and stay up to date on the latest.

We promise we won’t spam you! Just a monthly recap of our favorite wellness tips, updates and more.