Free shipping on all orders over $50 | Subscribe & save 15%
Free shipping on all orders over $50 | Subscribe & save 15%


Many new moms expect sleepless nights and endless diaper changes, but not burning, bladder pain, or that constant feeling of needing to pee. If you’ve noticed these symptoms while breastfeeding, you’re not alone and it’s definitely not “just in your head.”
A newer term called Genitourinary Syndrome of Lactation (GSL) is helping doctors better explain why bladder and vaginal discomfort are so common in breastfeeding women, and how it can sometimes make Interstitial Cystitis (IC) or Bladder Pain Syndrome (BPS) worse.
GSL refers to vaginal and urinary symptoms that happen during breastfeeding because of natural hormonal changes after giving birth. When you’re nursing, your body produces a hormone called prolactin to make milk. However, prolactin also lowers estrogen and testosterone levels, the very hormones that keep the vaginal, urethral, and bladder tissues thick, elastic, and well-lubricated.
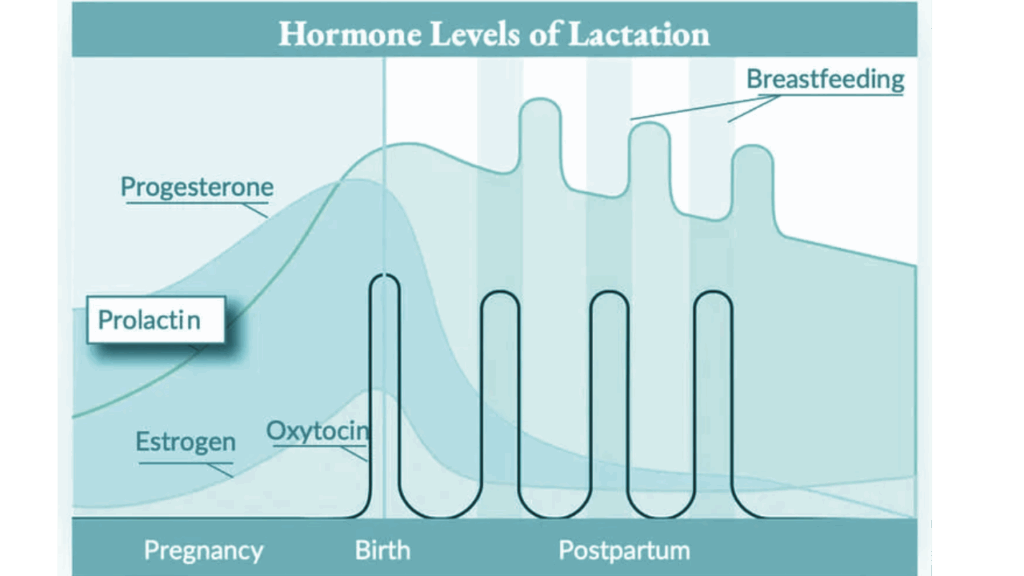
As these hormones drop, many women experience vaginal dryness or burning, pain with intercourse, low libido, bladder urgency or frequency, and a burning sensation during urination even when tests show no infection. Some women also report a constant feeling of irritation “down there.” Essentially, your tissues become more fragile and sensitive. Similar to what happens during menopause, but in younger women who are breastfeeding.
It’s not just hormone changes that cause discomfort. For several months after delivery, your pelvic floor muscles and nerves are also recovering from the strain of pregnancy and childbirth. Even if you had a cesarean section, bladder and vaginal symptoms are still common as your body heals. Women who don’t breastfeed may still experience these symptoms, but breastfeeding prolongs them by maintaining low levels of estrogen and testosterone.
If you have IC, you already know the telltale symptoms: bladder pressure, pain, urgency, and frequency without infection. Low estrogen levels during lactation can make these symptoms worse in several ways.
Estrogen helps keep the bladder lining strong and protective. When levels drop, the lining becomes thinner and more easily irritated, which means that normal things like urine acidity or certain foods can trigger pain. Low estrogen can also make the bladder nerves more sensitive, sending urgency and pain signals even when your bladder isn’t full.
Additionally, when vaginal or bladder tissues feel dry or sore, the pelvic floor muscles tend to tighten up as a protective response. Over time, this tension can increase bladder pain and worsen IC symptoms. GSL and IC often overlap, showing up as urgency, frequency, burning, and pelvic pain with negative urine cultures. That’s why many postpartum women are told they “just have a UTI” when the real issue is hormonal and structural.
If you’re breastfeeding and dealing with bladder or vaginal discomfort, there are safe and effective ways to feel better without needing to stop nursing.
Start by talking to your doctor or urogynecologist and explain that your symptoms began or worsened during breastfeeding. Mention both vaginal dryness and bladder irritation, since they’re often connected. Some women benefit from local estrogen therapy or a non-hormonal vaginal moisturizer. Low-dose vaginal estrogen creams, rings, or tablets can safely restore vaginal and urethral health even while breastfeeding, as they act locally with minimal absorption. Non-hormonal moisturizers can also help, while scented soaps or wipes should be avoided because they can worsen irritation. Non-hormonal supplements such as Femetry may be a helpful addition to your routine by supporting bladder comfort and microbiome balance while your hormones settle during lactation.

Pelvic floor physical therapy can also be beneficial. A pelvic floor therapist can teach you gentle exercises that help relax tight muscles, improve blood flow, and reduce pelvic or bladder pain. Limiting common bladder irritants such as caffeine, alcohol, carbonated drinks, and artificial sweeteners may also help reduce discomfort, especially when estrogen is low.
Finally, be patient and kind to yourself. These symptoms are common, hormonal, and treatable. You’re not doing anything wrong! Your body simply needs time, care, and support as it heals and adjusts postpartum.
